Abstract
Social determinants of health include the social and economic conditions that influence health status. Research into the impact of social determinants on individuals with type 2 diabetes has largely focused on the prevention of or risk of developing diabetes. No review exists summarizing the impact of social determinants of health outcomes in patients with type 2 diabetes. This systematic review examined whether social determinants of health have an impact on health outcomes in type 2 diabetes. Medline was searched for articles that (a) were published in English (b) targeted adults, ages 18 + years, (c) had a study population which was diagnosed with type 2 diabetes, (d) the study was done in the United States, and (e) the study measured at least one of the outcome measures—glycemic control, cholesterol (LDL), blood pressure, quality of life or cost. Using a reproducible strategy, 2,110 articles were identified, and 61 were reviewed based on inclusion criteria. Twelve were categorized as Economic Stability and Education, 17 were categorized as Social and Community Context, 28 were categorized as Health and Health Care, and three were categorized as Neighborhood and Built Environment. Based on the studies reviewed, social determinants have an impact on glycemic control, LDL, and blood pressure to varying degrees. The impact on cost and quality of life was not often measured, but when quality of life was investigated, it did show significance. More research is needed to better characterize the direct impact of social determinants of health on health outcomes in diabetes.
Similar content being viewed by others
Introduction
Social determinants of health include the social and economic conditions that influence health status [1]. As such, social determinants can be defined as the circumstances in which people are born, life, work, and age, as well as the systems set up to address illness [2]. This includes the economic and social gradient influenced by a broad set of conditions such as availability of resources to meet daily needs, access to educational, economic and job opportunities, access to health care services, availability of community-based resources and opportunities, transportation options, social support, and socioeconomic conditions [2]. A number of national and global organizations have developed frameworks to understand social determinants of health. Each framework organizes the key components into categories, establishing broad areas across multiple domains into one framework. Healthy People 2020 is an example of this framework, which was used to establish evidence-based resources, tools, and examples of addressing social determinants at the state and local level [2].
The relationship between social determinants of health and health outcomes has been established, but is not well understood [3–5]. Frameworks to conceptualize these influences generally indicate a bi-directional relationship between the individual and the socioeconomic and political context of their environment, with many mediating factors in between [6–8]. Studies have found associations among increased incidence, prevalence, and burden of disease with increasing levels of poverty and hunger, and lower levels of income, education, and socioeconomic status [3, 9–12]. In addition, studies have found differences in incidence, prevalence, and burden of disease by age, gender, race, and home circumstances [3, 9–12].
Increasingly, type 2 diabetes is being recognized as a condition upon which social determinants of health have a great impact [13]. Diabetes impacts more than 25.8 million people in the United States and 366 million people worldwide [14, 15]. While studies show the effectiveness of lifestyle-based diabetes interventions on improving individual outcomes, changes in diabetes outcomes at the population level have not followed. Insufficient attention to the essential role of social determinants of health has been suggested to explain this dichotomy [5, 13, 16–21]. Research into the impact of social determinants on individuals with type 2 diabetes has largely focused on the prevention of or risk of developing diabetes. International and domestic research suggests that social determinants such as income, education, housing, and access to nutritious food influence the development of type 2 diabetes [13, 21–27]. However, less evidence exists regarding the impact of social determinants of health on the progression of type 2 diabetes.
As no review exists summarizing the impact of social determinants on outcomes in patients with type 2 diabetes, this systematic review was conducted to answer whether social determinants of health have an impact on health outcomes in type 2 diabetes. To examine this, we focused on populations with type 2 diabetes and disease progression, rather than patients at risk of diabetes, and we examined multiple clinical and non-clinical outcomes including glycemic control, lipids, blood pressure, cost, and quality of life. The purpose of the review was to examine the impact of a broad range of social determinants, rather than limit the review to a specific subset. Given the current literature and the diverse topics, the Healthy People 2020 framework was used to select variables for analysis and categorize current knowledge on the impact of social determinants of health on outcomes for patients with type 2 diabetes.
Methods
Information sources, eligibility criteria and search
A reproducible strategy was used to identify studies investigating the impact of social determinants of health on outcomes in patients with type 2 diabetes. Studies were identified by searching Medline on May 29, 2013 for articles published in English between 2000 and 2013. A full description of the search terms and search process is shown in Table 1. This search was based on the comprehensive search conducted by Bambra et al. [28], investigating social determinants of health and health inequities. Some search terms were not used given the goals of this review to focus only on social determinants and not health inequities.
The following inclusion criteria were used to determine eligible study characteristics: (a) published in English, (b) targeted adults, ages 18 + years, (c) study population was diagnosed with type 2 diabetes, (d) the study was done in the United States, and (e) the study measured at least one of the outcome measures—glycemic control (HbA1c), cholesterol (LDL), blood pressure, quality of life or cost. The aforementioned clinical outcomes (HbA1c, LDL, and blood pressure) were chosen as required outcome measures because they are associated with successful self-care behaviors and lower rates of disease progression [13, 14]. Quality of life and cost was chosen as additional outcome measures because of the increasing demand for understanding the impact of diabetes to patients beyond classic clinical measures [14]. Quality of life is a well-accepted measure of general health status and can provide insight into the impact of complications and independent functioning. After adjusting for age and gender, average medical expenditures for patients with diabetes were shown to be 2.3 times higher than patients without diabetes [13]. Therefore, in addition to quality of life, cost can be an important consideration for the impact of social determinants of health on patients with type 2 diabetes.
Study selection and data collection
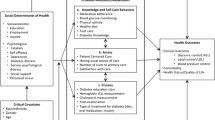
The process used to identify eligible citations is shown in Fig. 1. Titles were reviewed to ensure the study that targeted a population with type 2 diabetes. Articles were eliminated if they did not meet the study criteria, for instance, describing Type 1 diabetes, gestational diabetes, risk of developing diabetes, or diabetes prevention studies. Abstracts were then read and reviewed by four independent reviewers (RW, BS, JC, JW) using a standardized checklist for inclusion criteria to ensure all articles included of at least one outcome measure of interest. Finally, the abstracts and full articles were reviewed to determine which studies were conducted in the United States and to ensure the articles were focused on social determinants of health. We used the Healthy People definition of social determinants of health to determine if articles were focused on social determinants. Each article was placed in one of five categories (see Fig. 2) that described social determinants of health as related to economic stability, education, social and community context, health and health care, and, lastly, neighborhood and build environment [2]. Reviewers discussed any disagreement on inclusion or exclusion of articles and the senior topic expert (LE) weighed in as a fifth independent reviewer to help make the final decision regarding eligibility in the case of disagreement.
Data collected from the eligible articles are shown in Tables 2, 3, 4, and 5, where each table is specific to a social determinants category. Due to only one article being categorized as education, the economic stability and education categories were combined in the tables and discussion. Data were extracted for each article on the study design, study objective, number of participants, sample population, study setting, and the impact of the study on health outcomes (Tables 2, 3, 4, 5). The outcomes of interest measured, and statistical significance, if applicable, are noted in Table 6 for all categories. A narrative review was performed as the heterogeneous interventions and diverse study designs precluded conducting a meta-analysis. Though risk of bias exists, articles were not excluded due to the limited evidence available in the literature. The risk of bias across studies is discussed in the limitations, and the discussion gives more weight to studies using RCT design.
Results
Study selection
Figure 1 shows the results of the search. After duplicates were removed, the search resulted in 2,110 citations. After conducting a title review for type 2 diabetes populations producing 876 articles, an abstract review was done to ensure an outcome of interest was measured, resulting in 205 eligible studies conducted in the United States. Sixty-one eligible studies were identified based on the predetermined eligibility criteria and categorized into one of five Healthy People categories [29–89]. Twelve were categorized as Economic Stability and Education, 17 were categorized as Social and Community Context, 28 were categorized as Health and Health Care, and 3 were categorized as Neighborhood and Built Environment.
Study characteristics and outcomes of studies
Tables 2, 3, 4, and 5 provide a summary of the 61 studies that met eligibility criteria. Study designs included cross-sectional, retrospective cohort, randomized-controlled trials, path analysis, mixed methods, prospective cohort, and quasi-experimental. Sample sizes ranged from 30 to 148,846. Sample population and setting both varied substantially, as did impact on outcome.
Table 6 provides a summary of the outcomes measured and whether they were statistically significant. Across all 61 articles, 54 measured HbA1c, 18 measured LDL, 17 measured blood pressure, 6 measured cost, and 5 measured quality of life. Of these, 37 showed a significant association in HbA1c, 12 showed significance in LDL, 7 showed significance in blood pressure, 2 showed significance in cost, and 4 showed significance in quality of life. Within those categorized as Economic Stability and Education, 10 measured HbA1c, 5 of which were significant; 3 measured LDL, all of which were significant; 3 measured blood pressure, 2 of which were significant; 4 measured cost, 2 of which were significant; and no studies measured quality of life. Within those categorized as Social and Family Context, 14 measured HbA1c, 7 of which were significant; 5 measured LDL, 1 of which were significant; 4 measured blood pressure, 1 of which were significant; 1 measured cost, which was not significant; and 4 studies measured quality of life, 3 of which were significant. Within those categorized as Health and Health Care, all 28 measured HbA1c, 23 of which were significant; 10 measured LDL, 8 of which were significant; 10 measured blood pressure, 4 of which were significant; 1 measured cost, which was not significant; and no studies measured quality of life. Within those categorized as Neighborhood and Built Environment, 2 measured HbA1c, both of which were significant; no studies measured LDL, blood pressure, or cost; and 1 measured quality of life, which was significant.
Discussion
This systematic review is the first to synthesize the literature regarding the impact of social determinants of health on health outcomes in type 2 diabetes. Using a reproducible strategy, 2,110 articles were identified, and 61 were reviewed based on inclusion criteria. When categorizing by the Healthy People framework, studies tended to cluster into the Economic Stability, Social and Community Context, and Health and Health Care groups. Few studies investigated Education or Neighborhood and Built Environment. For the most part, studies were cross-sectional or cohort design, limiting the conclusions that can be made regarding causation. However, based on the studies reviewed, there is impact on glycemic control, LDL, and blood pressure to varying degrees. This suggests that social determinants of health have an influence on the progression of type 2 diabetes. The impact on cost and quality of life was not often measured, but when quality of life was investigated, it did show significance.
Summary of evidence by category
While care was taken to categorize and summarize studies included in the review, many articles were only tangentially related to social determinants of health. For example, many of the articles categorized as Economic Stability and Education were conducted in indigent populations, but the impact of their socioeconomic status was not taken into account. Kollannoor-Samuel et al. [61] found that those with lower socioeconomic status were more likely to have higher HbA1c, and a path analysis conducted by Kogan et al. [60] confirmed their hypothesis that financial distress, community disadvantage, and educational attainment demonstrated significant indirect effects on HbA1c through depressive symptoms. Considering the substantial evidence that exists linking increased diabetes incidence and prevalence to low socioeconomic status, more research is needed to determine the impact of Economic Stability and Education on diabetes outcomes.
Articles categorized as Social and Community Context considered topics such as depressive symptoms, health literacy, acculturation, race/ethnicity, gender, support resources, locus of control, and perceived control. Higher HbA1c was associated with low health literacy [70], acculturation [86], race [69], depressive symptoms [36], belief in chance [50], and social isolation [56]. However, these associations were not found across the board, with no significant relationships found in other studies investigating acculturation [68], social support resources [42], and depressive symptoms [43]. Higher quality of life was associated with lower depressive symptoms [40, 89] and higher perceived control [51]. Given the range of topics investigated and the varying degrees of association, Social and Community Context is an important influence to include when designing studies that take social determinants of health into consideration.
In the Health and Health Care category, many articles focused on the efficacy or effectiveness of a program, but often did not investigate the impact of health and health care access on the outcome. An impact on glycemic control was common, with 23 of the 28 showing statistically significant impact on HbA1c. Difficulty obtaining care, patients using acute care facilities, and no usual source of care were associated with higher HbA1c [74]. Harris et al. [49] found that with few exceptions, outcomes disparities between different racial groups did not differ significantly due to primary source of care, number of physician visits, or type of health insurance. Other aspects of health care, such as trust, were investigated, finding that patients with high trust were less likely to have poor glycemic control than those with lower trust [41].
Few studies investigated the impact of Neighborhood and Built Environment on diabetes outcomes. Seligman et al. found that those who were food insecure were more likely to have poor glycemic control in a sample of federally qualified health centers in the San Francisco Bay and Chicago areas [81]. Additionally, lower neighborhood SES was significantly associated with poorer physical and mental health [44]. Though, many authors have suggested that the neighborhood context plays a role in diabetes outcomes, this topic needs more evidence to fully understand its’ impact.
The Healthy People organizing framework was useful for categorizing articles related to social determinants of health and understanding what themes emerged in each broad area. It was challenging, however, to create mutually exclusive designations, especially if articles spanned multiple topics. As a result, it is possible that a different categorization scheme would help explain the evidence related to social determinants of health. Since the Healthy People framework was designed to create objectives for improving health and benchmarks for monitoring progress [2], this was a useful framework to inform how social determinants may need to be addressed at the national scale. Expanding research that consciously incorporates social determinants of health may, therefore, assist in both building an evidence base in the literature and informing national policy and legislation [13].
Summary of evidence by outcome
Glycemic control was the most commonly measured outcome, with 54 of the 61 articles measuring HbA1c and over half finding statistical significance. As glycemic control has been associated with lower rates of disease progression and fewer complications [14], this association is an important finding of the review. LDL and blood pressure were measured in roughly 1/3 of the articles, with 12 of the 18 showing statistical significance in LDL, and 7 of the 17 showing statistical significance in blood pressure. Most of the studies measuring these two outcomes were categorized in Health and Health Care. This suggests that social determinants related to health care access and technology can influence outcomes beyond glycemic control, and more investigation into other domains may be informative.
Cost and quality of life were rarely measured, with only 6 of the 61 measuring cost, and 5 of the 61 measuring quality of life. Five of the six studies measuring cost, and both of the 2 studies that found statistical significance in cost outcomes, were located in the category Economic Stability and Education. Conversely, the studies measuring quality of life were located in the Social and Community Context and Neighborhood and Built Environment categories, 4 of the 5 finding statistical significance. Considering the extensive search used and the lack of studies measuring these outcomes, more research is needed regarding the impact of social determinants of health on cost and quality of life. Additionally, these outcomes should be measured in studies across the domains, in order to inform how social determinants of health impact a wide range of health and functioning.
Limitations
There are four limitations to this study worth addressing. First, the search was limited to articles published in English between 2000 and 2013. Second, since studies with positive results are more likely to be published, the studies in this review may reflect publication bias. Third, the small number of RCTs and heterogeneous methodology prevented a meta-analysis from being performed. Finally, a majority of articles were observational designs, precluding the ability to comment on causation. Conclusions from this review are, therefore, qualitative and meant to guide future research rather than serve as conclusive answers.
Conclusion
Based on this review, social determinants may influence diabetes outcomes through an impact on glycemic control, though more investigation into other domains would be informative. More research is needed regarding the impact of social determinants of health on outcomes in type 2 diabetes. Specifically, more research should be focused on investigating the direct impact of social determinants of health on outcomes. Researchers should be careful to clearly define the health determinant of interest and ensure that the measure is deliberately being examined in studies. The impact of neighborhood environments must be explored further, as they are likely contributors to diabetes and diabetes-related outcomes. Also, the social determinants of the health literature must be strengthened, allowing for evidence useful in developing national policies for diabetes research and clinical care.
Further, social determinants of health are a poorly defined term that is used to describe an array of social, cultural, economic, demographic, psychosocial, and healthcare-related issues that may hinder an individual from achieving optimal health outcomes. In some research areas, studies are not labeled as being focused on social determinants of health but they may shed light on the subject area. In order to synthesize information on this topic area and draw meaningful conclusions, researchers must decide on terminology and/or fundamental categories of social determinants of health. In fact, this may be a vital piece in developing effective and efficient interventions in the future.
References
M. Marmot, Social determinants of health inequities. Lancet 365, 1099–1104 (2005)
Healthy People. Secretary’s Advisory Committee on Health Promotion and Disease Prevention Objectives for 2020. Healthy People 2020: An Opportunity to Address the Societal Determinants of Health in the United States. http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39
J. Bonnefoy, A. Morgan, M.P. Kelly, J. Butt, V. Bergman, Constructing the Evidence Base on the Social Determinants of Health: A Guide (The Measurement and Evidence Knowledge Network (MEKM) of the WHO Commission on Social Determinants of Health, Geneva, 2007)
M. Marmot, R. Wilkinson (eds.), Social Determinants of Health, 2nd edn. (Oxford University Press, Oxford, 2003)
A.S. Bierman, J.R. Dunn, Swimming upstream: access, health outcomes, and the social determinants of health. J. Gen. Internal. Med. 21(1), 99–100 (2006)
World Health Organization, Closing the gap: health equity through action on the social determinants of health (World Health Organization, Geneva, 2008)
Diderichsen F, Evans T, Whitehead M. The Social Basis of Disparities in Health, in Challenging inequities in health: from ethics to action, (Oxford, 2001), p 12
A.F. Brown, S.L. Ettner, J. Piette, M. Weinberger, E. Gregg, M.F. Shapiro, A.J. Karter, M. Safford, B. Waitzfelder, P.A. Prata, G.L. Beckles, Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol. Rev. 26, 63–77 (2004)
M. Kumari, M. Marmot, A. Rumley, G. Lowe, Social, behavioral, and metabolic determinants of plasma viscosity in the Whitehall II study. Ann. Epidemiol. 15(5), 398–404 (2005)
P.T. Martikainen, M.G. Marmot, Socioeconomic differences in weight gain and determinants and consequences of coronary risk factors. Am. J. Clin. Nutr. 69(4), 719–726 (1999)
M.G. Marmot, G.D. Smith, S. Stansfeld, C. Patel, F. North, J. Head, I. White, E. Brunner, A. Feeney, Health inequities among British civil servants: the Whitehall II study. Lancet 337(8754), 1387–1393 (1991)
M.G. Marmot, G. Rose, M. Shipley, P.J. Hamilton, Employment grade and coronary heart disease in British civil servants. J. Epidemiol. Community Health 32(4), 244–249 (1978)
Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, (Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, 2011)
International Diabetes Federation. IDF Diabetes Atlas, 5th edn. (International Diabetes Federation, Brussels, 2011), http://www.idf.org/diabetesatlas
J. Hill, M. Nielsen, M.H. Fox, Understanding the social factors that contribute to diabetes: a means to informing health care and social policies for the chronically ill. Permanente J. 17(2), 67–72 (2013)
L.C. Liburd, L. Jack, S. Williams, P. Tucker, Intervening on the social determinants of cardiovascular disease and diabetes. Am. J. Prev. Med. 29, 18–24 (2005)
D. Fry, S. Gleeson, C. Rissel, Health promotion and secondary prevention: response to Milat, O’Hara and Develin. Health Promot. J. Aust. 21(2), 86–91 (2010)
S.L. Maddigan, D.H. Feeny, S.R. Majumdar, K.B. Farris, J.A. Johnson, Understanding the determinants of health for people with type 2 diabetes. Am. J. Public Health 96(9), 1649–1655 (2006)
J. McKinlay, L. Marceau, US public health and the 21st century: diabetes mellitus. Lancet 356, 757–761 (2000)
L. Jack, L. Liburd, F. Vinicor, G. Brody, V.M. Murry, Influence of the environmental context on diabetes self-management: a rationale for developing a new research paradigm in diabetes education. Diabetes Educ. 25, 775–790 (1999)
Whiting D, Unwin V, Roglic G. Diabetes: equity and social determinants, in Equity, Social Determinants and Public Health Programs. (World Health Organization, Geneva, 2010), p 77
R. Dray-Spira, T.L. Gary-Webb, F.L. Brancati, Educational disparities in mortality among adults with diabetes in the US. Diabetes Care 33(6), 1200–1205 (2010)
E. Agardh, P. Allebeck, J. Hallqvist, T. Moradi, A. Sidorchuk, Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int. J. Epidemiol. 40(3), 804–818 (2011)
B.T. Smith, J.W. Lynch, C.S. Fox, S. Harper, M. Abrahamowicz, N.D. Almeida, E.B. Loucks, Life-course socioeconomic position and type 2 diabetes mellitus: the Framingham Offspring Study. Am. J. Epidemiol. 173(4), 438–447 (2011)
S.C. Maty, S.A. James, G.A. Kaplan, Life-course socioeconomic position and incidence of diabetes mellitus among blacks and whites: the Alameda County Study, 1965–1999. Am. J. Public Health 100(1), 137–145 (2010)
A.F. Andersen, C. Carson, H.C. Watt, D.A. Lawlor, K. Aylund, S. Ebrahim, Life-course socio-economic position, area deprivation and type 2 diabetes: findings from the British Women’s Health Study. Diabet. Med. 25(12), 1462–1468 (2008)
L.E. Egede, S. Dagogo-Jack, Epidemiology of type 2 diabetes: focus on ethnic minorities. Med. Clin. N Am. 89, 949–975 (2005)
C. Bambra, M. Gibson, A. Sowden, K. Wright, M. Whitehead, M. Petticrew, Tackling the wider social determinants of health and health inequities: evidence from systematic reviews. J. Epidemiol. Community Health 64, 284–291 (2010)
S.S. Bains, L.E. Egede, Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 13(3), 335–341 (2011)
N.A. Banister, S.T. Jastrow, V. Hodges, R. Loop, M.B. Gillham, Diabetes self-management training program in a community clinic improves patient outcomes at modest cost. J. Am. Diet. Assoc. 104(5), 807–810 (2004)
C.E. Bird, A.M. Fremont, A.S. Bierman et al., Does quality of care for cardiovascular disease and diabetes differ by gender for enrollees in managed care plans? Womens Health Issues 17(3), 131–138 (2007)
R. Bradley, E. Kozura, H. Buckle, J. Kaltunas, S. Tais, L.J. Standish, Description of clinical risk factor changes during naturopathic care for type 2 diabetes. J. Altern. Complement. Med. 15(6), 633–638 (2009)
P. Bray, D.M. Cummings, S. Morrissey et al., Improved outcomes in diabetes care for rural African Americans. Ann. Fam. Med. 11(2), 145–150 (2013)
F. Camacho, R.T. Anderson, R.A. Bell et al., Investigating correlates of health related quality of life in a low-income sample of patients with diabetes. Qual. Life Res. 11(8), 783–796 (2002)
K. Cavanaugh, K.A. Wallston, T. Gebretsadik et al., Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care 32(12), 2149–2155 (2009)
C.J. Chiu, L.A. Wray, E.A. Beverly, O.G. Dominic, The role of health behaviors in mediating the relationship between depressive symptoms and glycemic control in type 2 diabetes: a structural equation modeling approach. Soc. Psychiatry Psychiatr. Epidemiol. 45(1), 67–76 (2010)
D. Culica, J.W. Walton, E.A. Prezio, CoDE: community Diabetes Education for uninsured Mexican Americans. Proc (Bayl Univ Med Cent) 20(2), 111–117 (2007)
N. de Rekeneire, R.N. Rooks, E.M. Simonsick et al., Racial differences in glycemic control in a well-functioning older diabetic population: findings from the Health, Aging and Body Composition Study. Diabetes Care 26(7), 1986–1992 (2003)
E.D. Durden, B. Alemayehu, J.R. Bouchard, B.C. Chu, M. Aagren, Direct health care costs of patients with type 2 diabetes within a privately insured employed population, 2000 and 2005. J. Occup. Environ. Med. 51(12), 1460–1465 (2009)
L.E. Egede, C. Ellis, The effects of depression on metabolic control and quality of life in indigent patients with type 2 diabetes. Diabetes Technol Ther. 12(4), 257–262 (2010)
A. Fernandez, H. Seligman, J. Quan, R.J. Stern, E.A. Jacobs, Associations between aspects of culturally competent care and clinical outcomes among patients with diabetes. Med. Care 50(9 Suppl 2), S74–S79 (2012)
A.L. Fortmann, L.C. Gallo, A. Philis-Tsimikas, Glycemic control among Latinos with type 2 diabetes: the role of social-environmental support resources. Health Psychol. 30(3), 251–258 (2011)
T.L. Gary, R.M. Crum, L. Cooper-Patrick, D. Ford, F.L. Brancati, Depressive symptoms and metabolic control in African-Americans with type 2 diabetes. Diabetes Care 23(1), 23–29 (2000)
T.L. Gary-Webb, K. Baptiste-Roberts, L. Pham et al., Neighborhood socioeconomic status, depression, and health status in the Look AHEAD (Action for Health in Diabetes) study. BMC Public Health 11, 349 (2011)
E.M. Geraghty, T. Balsbaugh, J. Nuovo, S. Tandon, Using geographic information systems (GIS) to assess outcome disparities in patients with type 2 diabetes and hyperlipidemia. J. Am. Board Fam. Med. 23(1), 88–96 (2010)
R. Gold, K. Yu, L.J. Liang et al., Synchronous provider visit and self-management education improves glycemic control in Hispanic patients with long-standing type 2 diabetes. Diabetes Educ. 34(6), 990–995 (2008)
R.W. Grant, E. Cagliero, H.C. Chueh, J.B. Meigs, Internet use among primary care patients with type 2 diabetes: the generation and education gap. J. Gen. Intern. Med. 20(5), 470–473 (2005)
R.W. Grant, N.G. Devita, D.E. Singer, J.B. Meigs, Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care 26(5), 1408–1412 (2003)
M.I. Harris, Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care 24(3), 454–459 (2001)
R.P. Hayes, A.M. Bernard, W. Slocum et al., Diabetes in urban African Americans: assessment of diabetes-specific locus of control in patients with type 2 diabetes. Diabetes Educ. 26(1), 121–128 (2000)
M.A. Hernandez-Tejada, C.P. Lynch, J.L. Strom, L.E. Egede, Effect of perceived control on quality of life in indigent adults with type 2 diabetes. Diabetes Educ. 38(2), 256–262 (2012)
F. Hill-Briggs, T.L. Gary, L.R. Bone, M.N. Hill, D.M. Levine, F.L. Brancati, Medication adherence and diabetes control in urban African Americans with type 2 diabetes. Health Psychol. 24(4), 349–357 (2005)
F. Hill-Briggs, M. Lazo, M. Peyrot et al., Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J. Gen. Intern. Med. 26(9), 972–978 (2011)
J.M. Jakicic, C.M. Egan, A.N. Fabricatore et al., Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the look AHEAD trial. Diabetes Care 36(5), 1297–1303 (2013)
K.A. Johnson, S. Chen, I.N. Cheng et al., The impact of clinical pharmacy services integrated into medical homes on diabetes-related clinical outcomes. Ann. Pharmacother. 44(12), 1877–1886 (2010)
G. Kacerovsky-Bielesz, S. Lienhardt, M. Hagenhofer et al., Sex-related psychological effects on metabolic control in type 2 diabetes mellitus. Diabetologia 52(5), 781–788 (2009)
M.A. Khan, S. Shah, A. Grudzien et al., A diabetes education multimedia program in the waiting room setting. Diabetes Ther. 2(3), 178–188 (2011)
J.K. Kirk, S.W. Davis, C.A. Hildebrandt, E.N. Strachan, M.L. Peechara, R. Lord, Characteristics associated with glycemic control among family medicine patients with type 2 diabetes. N C Med. J. 72(5), 345–350 (2011)
D.E. Knight, R.W. Draeger, P.C. Heaton, N.C. Patel, Pharmacist screening for depression among patients with diabetes in an urban primary care setting. J. Am. Pharm. Assoc. (2003) 48(4), 518–521 (2008)
S.M. Kogan, G.H. Brody, Y.F. Chen, Depressive symptomatology mediates the effect of socioeconomic disadvantage on HbA(1c) among rural African Americans with type 2 diabetes. J. Psychosom. Res. 67(4), 289–296 (2009)
G. Kollannoor-Samuel, J. Chhabra, M.L. Fernandez et al., Determinants of fasting plasma glucose and glycosylated hemoglobin among low income Latinos with poorly controlled type 2 diabetes. J. Immigr. Minor. Health 13(5), 809–817 (2011)
D.R. Lairson, S.J. Yoon, P.M. Carter et al., Economic evaluation of an intensified disease management system for patients with type 2 diabetes. Dis Manag. 11(2), 79–94 (2008)
B.K. Lind, W.E. Lafferty, D.E. Grembowski, P.K. Diehr, Complementary and alternative provider use by insured patients with diabetes in Washington State. J. Altern. Complement Med. 12(1), 71–77 (2006)
B. Littenberg, C.D. MacLean, L. Hurowitz, The use of adherence aids by adults with diabetes: a cross-sectional survey. BMC Fam. Pract. 7, 1 (2006)
M.L. McPherson, S.W. Smith, A. Powers, I.H. Zuckerman, Association between diabetes patients’ knowledge about medications and their blood glucose control. Res. Social Adm. Pharm. 4(1), 37–45 (2008)
C.D. Miller, C.S. Barnes, L.S. Phillips et al., Rapid A1c availability improves clinical decision-making in an urban primary care clinic. Diabetes Care 26(4), 1158–1163 (2003)
C.K. Miller, J.L. Kristeller, A. Headings, H. Nagaraja, W.F. Miser, Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr. Diet. 112(11), 1835–1842 (2012)
N. Moayad, H. Balcazar, V. Pedregon, L. Velasco, M. Bayona, Do acculturation and family cohesiveness influence severity of diabetes among Mexican Americans? Ethn. Dis. Spring. 16(2), 452–459 (2006)
I.S. Okosun, G.E. Dever, Abdominal obesity and ethnic differences in diabetes awareness, treatment, and glycemic control. Obes. Res. 10(12), 1241–1250 (2002)
C.Y. Osborn, S.S. Bains, L.E. Egede, Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. 12(11), 913–919 (2010)
R. Otero-Sabogal, D. Arretz, S. Siebold et al., Physician-community health worker partnering to support diabetes self-management in primary care. Qual. Prim. Care. 18(6), 363–372 (2010)
W. Polonsky, L. Fisher, C. Schikman et al., The value of episodic, intensive blood glucose monitoring in non-insulin treated persons with Type 2 Diabetes: design of the Structured Testing Program (STeP) study, a cluster-randomised, clinical trial [NCT00674986]. BMC Fam. Pract. 11, 37 (2010)
S.A. Quandt, R.A. Bell, B.M. Snively et al., Ethnic disparities in glycemic control among rural older adults with type 2 diabetes. Ethn Dis. Autumn. 15(4), 656–663 (2005)
M.K. Rhee, C.B. Cook, V.G. Dunbar et al., Limited health care access impairs glycemic control in low income urban African Americans with type 2 diabetes. J. Health Care Poor Underserved 16(4), 734–746 (2005)
H.W. Rodbard, A.J. Green, K.M. Fox, S. Grandy, Impact of type 2 diabetes mellitus on prescription medication burden and out-of-pocket healthcare expenses. Diabetes Res. Clin. Pract. 87(3), 360–365 (2010)
R. Rothman, R. Malone, B. Bryant, C. Horlen, M. Pignone, Pharmacist-led, primary care-based disease management improves hemoglobin A1c in high-risk patients with diabetes. Am. J. Med. Qual. 18(2), 51–58 (2003)
V. Ruelas, G.M. Roybal, Y. Lu, D. Goldman, A. Peters, Clinical and behavioral correlates of achieving and maintaining glycemic targets in an underserved population with type 2 diabetes. Diabetes Care 32(1), 54–56 (2009)
L. Ruggiero, A. Moadsiri, P. Butler et al., Supporting diabetes self-care in underserved populations: a randomized pilot study using medical assistant coaches. Diabetes Educ. 36(1), 127–131 (2010)
M.C. Salvo, A.M. Brooks, Glycemic control and preventive care measures of indigent diabetes patients within a pharmacist-managed insulin titration program vs standard care. Ann. Pharmacother. 46(1), 29–34 (2012)
J.M. Schectman, M.M. Nadkarni, J.D. Voss, The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care 25(6), 1015–1021 (2002)
H.K. Seligman, E.A. Jacobs, A. Lopez, J. Tschann, A. Fernandez, Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care 35(2), 233–238 (2012)
T.L. Smith, M.L. Drum, J. Miernik, L.A. Fogelfeld, R.B. Lipton, Early and later onset type 2 diabetes in uninsured patients: clinical and behavioral differences. J. Health Care Poor Underserved 19(4), 1119–1135 (2008)
M.S. Spencer, A.M. Rosland, E.C. Kieffer et al., Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am. J. Public Health 101(12), 2253–2260 (2011)
M.W. Strum, R. Hopkins, D.S. West, B.N. Harris, Effects of a medication assistance program on health outcomes in patients with type 2 diabetes mellitus. Am. J. Health Syst. Pharm. 62(10), 1048–1052 (2005)
D.J. Toobert, R.E. Glasgow, L.A. Strycker, M. Barrera Jr, D.P. Ritzwoller, G. Weidner, Long-term effects of the Mediterranean lifestyle program: a randomized clinical trial for postmenopausal women with type 2 diabetes. Int J Behav Nutr Phys Act. 4, 1 (2007)
S. Venkatesh, L.J. Weatherspoon, S.A. Kaplowitz, W.O. Song, Acculturation and glycemic control of Asian Indian adults with type 2 diabetes. J. Community Health 38(1), 78–85 (2013)
P.E. Wandell, C. Gafvels, Patients with type 2 diabetes aged 35–64 years at four primary health care centres in Stockholm County, Sweden. Prevalence and complications in relation to gender and socio-economic status. Diabetes Res. Clin. Pract. 63(3), 195–203 (2004)
G. Welch, N.A. Allen, S.E. Zagarins, K.D. Stamp, S.E. Bursell, R.J. Kedziora, Comprehensive diabetes management program for poorly controlled Hispanic type 2 patients at a community health center. Diabetes Educ. 37(5), 680–688 (2011)
D.J. Wexler, R.W. Grant, E. Wittenberg et al., Correlates of health-related quality of life in type 2 diabetes. Diabetologia 49(7), 1489–1497 (2006)
Acknowledgment
This study was supported by grant 5K24DK093699-02 National Institute of Diabetes and Digestive Kidney Disease (NIDDK). The funding agency did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The manuscript represents the views of the authors and not those of the VA or HSR&D.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walker, R.J., Smalls, B.L., Campbell, J.A. et al. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine 47, 29–48 (2014). https://doi.org/10.1007/s12020-014-0195-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0195-0